Douglas Ebersole, MD
April 2020
I come to you as a recreational and technical diving instructor, as a physician consultant for Divers Alert Network, and as a COVID-19 survivor. For me, was just an occupational hazard. I tested positive for COVID-19 after seeing a patient in my cardiology clinic for an unrelated condition who seemed quite short of breath. He was admitted to the ICU and tested positive for COVID-19. Thankfully, he did not require a ventilator and recovered after approximately two weeks in the hospital. I was notified of his positive test one week after my exposure. As I had been wearing my N95 mask when I saw him, I was advised to take my temperature daily and self monitor for symptoms. I did well for a few days and then began developing a cough and profound fatigue followed by fever. I ended up testing positive and spent the next couple of weeks quarantined at home. I have now recovered and will be going back to work this week and look forward to returning to diving. More on that later. I am definitely one of the lucky ones. Thousands of others have been hospitalized, required ventilators, and have died. Our thoughts and prayers should go out to those patients and their families.
While this is a horrific global event, the diving industry will come out the other side. When we do, how do we safely get people diving? This is a multifactorial issue, involving dive shops, dive charters, instructors, and the individual diver/student.
Background
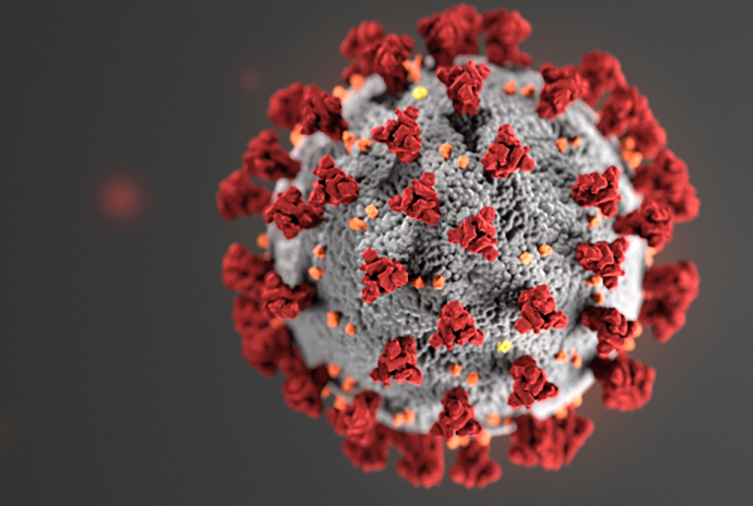
The novel coronavirus, known as SARS-CoV-2, is the cause of the disease COVID-19 which has killed almost 200,000 people worldwide as of today (April 25, 2020). SARS-COvV-2 is part of the viral group known as “corona” (Latin for “crown” or “halo”) because of the pattern of proteins that stud its surface. Coronaviruses are responsible for 15-30% of acute respiratory infections each year. Human to human spread of the virus is by way of large respiratory droplets (coughing, sneezing, speaking) and touching contaminated surfaces. The incubation period of the virus is 2-14 days with a mean of 5.1 days.
Medical experts believe a vaccine for COVID-19 is still at least 18 months away. Until a vaccine is available or effective therapies are found, the disease will continue to spread. The impact of social distancing and “flattening the curve” has been helping keep people safe and helping to avoid overwhelming our medical resources, but it has also had a massive economic impact on society. This impact has been felt especially severe in the diving industry as it is based on discretionary spending by consumers. Additionally, for many divers, their interest in diving is strongly linked to the ability to travel internationally. Until travel restrictions are lifted and consumers are confident in the ability of the airlines and cruise industry to keep them safe, the dive industry will likely continue to suffer economically. But enough doom and gloom. What can we do as a community to help the dive industry?
Dive Centers
The diver or dive student needs to feel safe before they will go into a store to purchase gear or training, to board a dive charter, or simply to go diving. For the foreseeable future, this is going to mean wearing masks in public, social distancing in dive shops, fewer passengers spread out on dive charters, an emphasis on online training where possible, and smaller class sizes, again to allow students to practice social distancing. Pay by phone or curbside tank drop off could also be effective interventions to reduce the chance of infection.
One positive aspect of this pandemic is it has forced dive shops and training agencies to move towards more online training. E-learning has been growing in popularity for some time and has been embraced by various training agencies and dive centers to greater and lesser degrees. RAID now allows students access to all of their training materials from open water diver through cave diving instructor at no cost. Other training agencies have also moved towards offering certain courses at low or no cost to students in an attempt to keep money flowing into the dive centers during this very difficult time.
Webinars and Zoom conferences have become the new normal. There have been a number of outstanding live conferences put on by The Diver Medic, Dirty Dozen Expeditions, Dive Ninjas, Deeper Discussions and Shallow Thoughts, Divesoft Talk Live, and many others these past few weeks. I imagine dive centers will incorporate this mode of education into some aspects of their academic courses in the future.
Unfortunately, many dive centers will not be able to financially weather this storm, but as a community we need to do everything we can to help support our local dive centers. Take this time out of the water to get your gear serviced. For dive centers not located in diving hotspots like Florida or California, it is going to be really tough until travel restrictions are lifted and their customers feel comfortable getting on an airplane. If you have a trip that is in jeopardy, consider rescheduling rather than cancelling and asking for a refund. Buy gear in preparation for upcoming dive trips in advance of the quarantines and shelter in place orders being lifted. Sign up for continuing education and do the academic portions online or via a conferencing app with your instructor. Every little bit helps. We are all in this together.
Gear Cleaning
Rinsing off dive gear at the end of each pool session will no longer suffice. We need to truly disinfect any items that could be shared among divers, especially regulators and BCDs.
Divers Alert Network (DAN) has recently published guidelines regarding disinfecting scuba gear. The link is here:
Coronaviruses belong to a group of enveloped viruses, which means the virion (the form that the virus takes while outside the host cell) is protected by an oily lipid layer. As with most enveloped viruses, damaging or destroying this lipid layer will inactivate the virus. Studies of other coronaviruses have shown their infectivity can be reduced by heat, UV light and alkaline or acidic conditions. Because of this, and the fact that enveloped viruses are generally easily inactivated, surfaces can be disinfected using household cleaning products.
Because research into SARS-CoV-2 is ongoing, there is debate about how long it can survive on surfaces. Recent studies have shown that it can survive up to 3 hours in an aerosol droplet (such as from a sneeze), 4 hours on copper, 24 hours on cardboard, and 2-3 days on plastic and stainless steel. In water, however, it is unclear how long SARS-CoV-2 survives. Studies on the SARS virus, called SARS-CoV-1 and the cause of an epidemic in 2003, have shown that it remained infectious for long periods in surface water (lakes, rivers, wetlands, etc.) and previously pasteurized sewage at both low and ambient temperatures. In chlorinated or bromated pools and hot tubs, the CDC specifies that SARS-CoV-2 would be inactivated.
Heat
There is very little data on SARS-CoV-2, and much of it is preliminary. In times like these scientists will look to related but slightly harder-to-kill viruses. In the case of the novel coronavirus, some data reports are based on the SARS-CoV-1 virus because it is more difficult to kill than the novel coronavirus. One study found that the SARS-CoV-1 virus loses infectivity after being heated to 133°F (56°C) for 15 minutes, and the World Health Organization specifies this temperature and timing as well . Another study found that the SARS-CoV-1 virus remains stable between 40°F (4°C) and 98°F (37°C) and would lose infectivity after 30 minutes at 133°F (56°C).
Divers Alert Network has received questions about the virus entering a scuba cylinder as a result of contaminated air being drawn into the compressor. During the process of compressing air, using the ideal gas equation T2 = T1 x (P2/P1)(n-1)/n we can calculate that a four-stage compressor with 1 ATA inlet pressure and an 80°F environment pumping air up to 29 ATA or around 4000 psi, would have an inter-stage temperature inside the cylinder of 224 °F. This calculation is very basic and does not account for anything outside of ideal conditions. However, it does indicate the instantaneous temperature at the moment of peak pressure.
In reality, the outlet valve temperature will likely be 170°F-190°F, and the gas temperature around 150°F, occurring during each stage of the compressor (i.e. four cycles for a four-stage compressor assuming each stage’s outlet temperature is the same). Because this is definitively hot enough to kill SARS-CoV-2, it is therefore unlikely that COVID-19 would survive this process should an infected individual cough into the compressor intake. It is important to note that infected droplets exhaled by a person can be as small as 0.5 micron; the filter systems alone would not remove these, but the virus should be dead at that stage.
It should be noted, however, that if an individual carried the virus on their hands, either as a result of being infected or unknowingly touching an infected surface, and touches the cylinder valve or fill whip, the virus could potentially enter the cylinder through this route. It has been shown that some viruses are extremely pressure resistant — an order of magnitude above diving gas storage pressures. These studies, however, were conducted on noroviruses, a non-enveloped group of viruses that are generally harder to kill than enveloped viruses. Other studies conducted on enveloped viruses such as the flu only explored the efficacy of high hydrostatic pressure at 289.6 MPa (42,003 PSI) . It is therefore very important to practice hand washing and disinfection of high-touch areas including cylinders and fill stations, as it is likely that a virus could survive at diving gas storage pressures.
EPA Guidelines
No matter the active ingredient or method of disinfecting scuba equipment, proven efficacy against the novel coronavirus is of utmost importance. The EPA’s “List N” is a compilation of products that have proven efficacy against SARS-CoV-1 and will therefore also work to kill SARS-CoV-2. Outside of the United States, local governing bodies may also have registered disinfectants. Following the directions for use for each individual product will ensure its efficacy.

When product manufacturers register their products with the EPA, they must submit a list of uses for the product. It is uncommon for registered products on List N to contain “scuba”; more likely to be listed are respirators or materials that scuba equipment is made of. When choosing a disinfectant solution from List N it is important to check that the product’s EPA registration specifies its use for the materials in question.
Some products commonly recommended by underwater breathing equipment manufacturers are classified as quaternary ammonium sanitizers registered with the EPA for use in food service only and are not currently on the EPA’s List N. The EPA does not consider them to be effective against SARS-CoV-2 when applied on those materials and surfaces.

Quaternary Ammonium Compounds
Quaternary ammonium compounds, or quats, are a group of chemicals that are exceedingly common as active ingredients in cleaning solutions. These agents are hydrophobic and as such are effective against enveloped viruses. Quats are thought to react with the viral envelope and “disorganize” it, leading to the contents of the virus leaking out and degrading. In addition, little evidence exists to support viral resistance against these compounds. Studies have shown that quats are effective against SARS-CoV-1, and the World Health Organization (WHO) recommends the use of cleaning products containing these compounds in their laboratory biosafety guidance related to coronavirus disease 2019.
Simple Green has been shown to be effective against viruses similar to SARS-CoV-2 when used in accordance to its directions for use.

While not on the List N , another agent that has been shown to be effective against SARS-CoV-1 is MadaCide-1. It’s labeling states that it is effective against the SARS-CoV-1 virus if used with a contact time of two minutes and other viruses such as Hepatitis B and Hepatitis C with five minutes of contact time.
While Steramine is an effective sanitizing product, and some manufacturers recommend it for use on dive gear, it does not appear on the EPA's “List N” and is thus not endorsed for removal of the new coronavirus.
Bleach
Bleach, or sodium hypochlorite, has been studied in many different concentrations, and its effectiveness against viruses has been proven. It is a strong oxidant that works by damaging the viral genome. According to the WHO, the recommended bleach solution for general disinfection is a 1:100 dilution of 5% sodium hypochlorite. (Note that some brands of bleach have different concentrations of the active ingredient, such as those that are thickened and marketed to reduce splashing.)
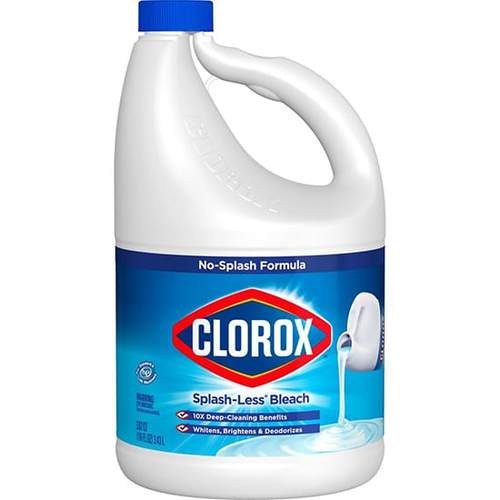
This dilution yields 0.05% or 500 ppm of the active ingredient and requires a soaking time of 30 minutes if objects are immersed in the solution or at least 10 minutes if sprayed onto a nonporous surface. In a study that examined SARS-CoV-2 specifically, it was found that a bleach concentration of 0.1% or 1,000 ppm was needed to reduce infectivity when sprayed onto a hard-non-porous surface. A second study on the same virus found that 0.1% sodium hypochlorite would inactivate the virus within 1 minute. A study on SARS-CoV-1 found that both 1:50 (0.1%) and 1:100 (0.05%) inactivated the virus after an immersion of 5 minutes.
When using bleach, the use of gloves, a mask, and eye protection is encouraged. Mix the solutions in well-ventilated areas, and use cold water, as hot water will decompose the active ingredient. It is important to never mix bleach with other chemicals and to remove all organic matter from items to be disinfected, as this too will inactivate the active ingredient. Items disinfected with bleach must be thoroughly rinsed with fresh water and allowed to dry before use, as it is corrosive to stainless steel (in higher concentrations) and irritating to mucous membranes, skin and eyes. Highly concentrated bleach solutions have also been found to be harmful to life-support equipment, causing metal fatigue and in some cases hose failure during the Hart building anthrax attack. As such these solutions are not used by EPA units for dive equipment when effective alternatives exist.
Soap and Water
Washing hands and surfaces with soap and water is one of the most effective ways to protect against the virus. The type of soap used is not important. Washing with soap and water does not kill microorganisms but physically removes them from a surface. Running water by itself can be effective in removing some unwanted material from surfaces, however, soap will physically pull material from the skin and into the water. Divers Alert Network was asked why soap and water will not work for scuba equipment if it is recommended for hands. Soap and water, as stated above, must be combined with mechanical action to be completely effective. Soaking scuba equipment in soapy water alone is not an effective disinfection method. If soapy water was combined with mechanical action, it would theoretically prove to be more efficient. However, there are some parts of scuba equipment that are not easily reached without disassembly, such as the inside of a regulator. Since an exhaled breath will travel through the inside of a regulator and make contact with the diaphragm, lever arm, and other internal surfaces, soaking the regulator in a disinfectant solution may be a better option.
Best Practices
When selecting a disinfectant, it is of utmost importance to use a product that has proven efficacy against either SARS-CoV-2 or the harder-to-kill SARS-CoV-1. Consult your local governing body’s pesticide registration system for its list of registered disinfectants if the products specified in the EPA’s List N are unavailable in your area. When using these products, be sure to follow the directions and use the specified personal protective equipment (such as gloves or eye protection) when disinfecting. If registered products cannot be found, be sure to use disinfection protocols outlined by the CDC.
To disinfect equipment to kill the virus that causes COVID-19, a disinfectant on the EPA's List N should be used. Before using a product, check to see if it has been registered with the EPA for use on dive equipment, respirators or the materials these are made of. Alternatively, the CDC recommends a 4:100 bleach solution (1/3 cup of bleach in 1 gallon of water) with a contact time of 1 minute.
After disinfecting equipment, one must take care not to re-infect the equipment, such as by handling it when storing. Dive shop employees should take care to maintain good hygiene by washing hands frequently and regularly disinfecting high-touch areas, including fill stations (as outlined in the “heat” section of this article).
When using any disinfectant, be sure to follow the manufacturer's instructions for use. Follow this with a thorough rinse in fresh water, and allow the equipment to dry completely before use.
Finally, consider updating your existing emergency action plan to include a potential COVID-19 infection by staff or customers. Be sure to outline all disinfection protocols and ensure that they are being diligently followed by all staff. The most important consideration is the health and safety of your staff and customers.
Divers Alert Network (DAN) has also issued some advice regarding protecting divers when they travel—and especially with respect to renting gear.
DAN states: “Equipment can be effectively sanitized by submerging it in a 10% bleach solution or using a cleaning product such as Steramine tablets or any other quaternary ammonium compound. Be sure to use these products according to the manufacturer’s directions and then rinse the gear with fresh water.
“Products that are commonly used to clean dive gear but are ineffective against coronavirus include antibacterial and chlorhexidine mouthwashes or sprays. Hot soapy water must be paired with mechanical action such as scrubbing with a soft toothbrush to be effective.”
If you’re traveling and using rental gear, DAN suggests using a “household disinfecting wipe” to clean your regulator mouthpiece, snorkel, BCD oral inflator and the inside of your mask, and then rinsing with fresh water before use. DAN advises you to ask your operator to sanitize the equipment you’re renting—if you don’t have access to wipes to do it yourself.
Dive Training
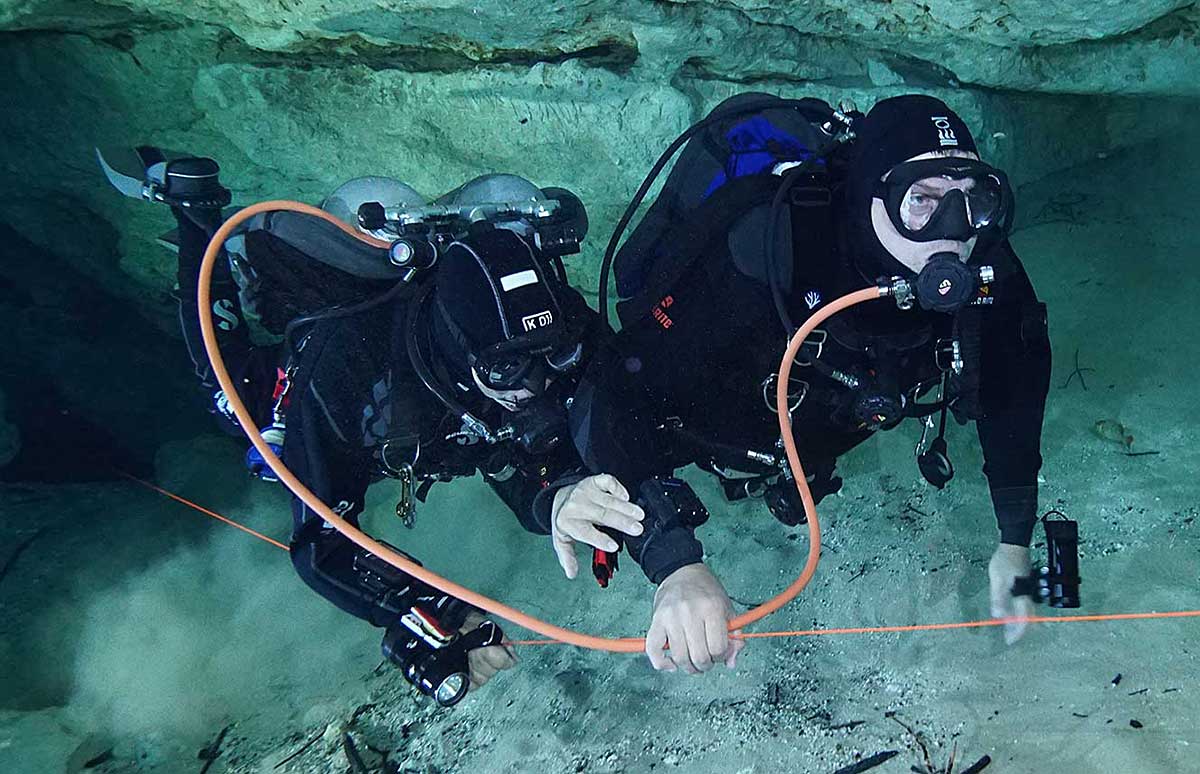
The main issue with training divers is how do we effectively teach them the important skill of air-sharing without potentially putting their health at risk. Training agencies require students to demonstrate in-water “air-sharing” exercises to meet general standards published by the various diving standards organizations. Widespread concerns surrounding the novel coronavirus and COVID-19 infection have demanded we allow changes to the way this skill is demonstrated and practiced during both confined skills training and open water certification dives.
Since RAID has a mandatory S-Drill and is a “primary” gas-sharing agency, cross-contamination is impossible to reduce. Therefore, RAID has designed a new protocol that, with only a minor change, will still meet the requirements for certification. Other agencies are considering similar changes in their training standards.
In simplified terms, to demonstrate a classic air-sharing drill, one diver gives their buddy an out-of-air (OOA) signal, their buddy donates their primary regulator second stage, and the diver simulating OOA places it into their mouth and breathes from it.
Under present circumstances, this method could present an opportunity for cross-infection, not just in chlorinated swimming pool water but also, certainly, in freshwater or the open ocean.
In the interests of diver and instructor safety, and until further notice, RAID is asking its members to follow this revised protocol for S-Drills and in-place OOA simulations.
- Drill begins
- Diver one, simulating OOA, signals their buddy, “Out of Air!”
- Diver two presents a working second-stage regulator.
- Diver one takes the offered regulator and switches from their primary regulator to their backup second stage while gently purging the donated second stage to check that it is working.
- All the steps from a normal air-sharing drill are practiced – only the switch to the buddy’s regulator is simulated.
- When the drill is completed (after horizontal swim, ascent, etc.), diver one returns the donated regulator to their buddy.
This method adequately demonstrates all of the component skills of an air-sharing drill, including having the OOA diver switch regulators without exposing either diver to an elevated risk of cross contamination.
Returning to Diving after COVID-19
What about the diver, like myself, who has contracted COVID-19? When can they safely return to diving? Unfortunately, the answer to that question is not known at the present time, but is not likely to be a “one size fits all” answer.
Like with any illness, the diver will need to completely resolve their symptoms and have good exercise tolerance before even considering a return to diving. However, COVID-19 in some cases aggressively attacks the pulmonary and cardiovascular system and the duration of these effects is unknown, but likely highly variable among individuals.
COVID-19 (SARS-COV-2) is a coronavirus and is similar to, though not exactly like, the coronavirus (SARS-COV-1) that caused SARS (severe acute respiratory syndrome). As we don’t have a great deal of long term data yet on COVID-19, looking at the longer term effects from SARS-COV-1 may be helpful in making recommendations for divers until we have better data on COVID-19.
A study of the pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome (SARS) was reported in the European Respiratory Journal in 2004. They looked at 46 survivors of SARS 3 months after hospital discharge. (Eur Repsir J 2004:24:436-442). No abnormalities were detected in the pulmonary function tests in 23 (50%) of the patients. Abnormalities of forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FEV1/FVC and TLCO were detected in seven (15%), 12 (25%), one, (2%), and 18 (39%) of patients, respectively. All of these abnormalities were mild except in one case. Breathing reserve was low in four patients and significant oxygen desaturation was detected in another four patients. Comparison of the measured exercise capacity with resting pulmonary function tests showed many cases of discordance in impairment. They concluded that pulmonary function defects were detected in half of the recovered severe acute respiratory syndrome patients 3 months after hospital discharge, but the impairment was mild in almost all cases. Many patients had reduced exercise capacity that could not be accounted for by the impairment in pulmonary function.
Recently, a preliminary report from Frank Hartig, a senior physician at the Innsbruck University Clinic in Austria, was published in the dive magazine “Wetnotes” and an English translation was posted on Facebook. Dr. Hartig is an avid diver and heads the emergency department in the hospital and is responsible for coordinating the care of their COVID-19 patients. He reports having treated dozens of COVID-19 patients in recent weeks, six of whom were divers. All six of these divers did not require hospitalization and felt as though they had recovered from their illness 5-6 weeks earlier. However, two of the patients showed hypoxemia under stress, two demonstrated reactive airway disease, and four showed “impressive” lung changes on CT scans. The English translation reported “the damage to the lungs is irreversible”’ though the follow-up tests only occurred approximately six weeks after clinical resolution of symptoms.
We must interpret this small case series with caution for now while awaiting further data. It is definitely interesting, quite thought provoking, and is hypothesis generating for future research. However, it is only six divers and is very short follow-up. It is, however, a good reason to pause and consider how to decide when to return to diving after being infected with COVID-19. We just need to wait for larger, more controlled studies with longer follow up before becoming overly concerned and making sweeping changes to evaluation of fitness to dive protocols around the world.
The Undersea and Hyperbaric Medical Society put out a position paper on their website (www.uhms.org) on April 24, 2020. They agree that at the present time, we simply do not have sufficient data to support or refute the proclamations made by the case series from Dr. Hartig. They feel the list of potential variables related to how this disease manifests, its clinical course, and long-term prognosis is lengthy and may include factors such as underlying medical conditions, age, disease severity, and secondary complications. Case reports suffer from multiple design weaknesses to include a lack of controls and randomization, which makes any conclusions that we may want to generalize to a larger population suspect. While these findings are indeed disquieting, it will take time before the potential impact on individual health, and any lasting effects on lung or heart function, are captured in the peer-reviewed literature.
A position paper by the Belgian Society for Diving and Hyperbaric Medicine was published on April 12, 2020 in an attempt to provide guidelines to physicians evaluating divers who have suffered COVID-19. Click here for their recommendations
April 12, 2020
The COVID-19 pandemic has had a major impact on recreational and professional diving activities, with an almost complete cessation of this activity during many weeks/months. These measures were a logical consequence of Government and Public Health Care recommendations to limit unnecessary commuting but also because it is virtually impossible to observe the regulations of “social distancing” and avoiding the possible sharing of divers’ breathing equipment. Lastly, there is a real possibility that emergency first aid teams may be overwhelmed by cases related to COVID-19 or the logistics involved (decontamination procedures), and not be able to respond in a timely and efficient manner.
When the precautionary measures to combat the pandemic will be relaxed, it is important to resume normal recreational and professional diving activities as soon as reasonably possible, both for the social, physical and mental welfare of the diving population. The question has been raised, whether having suffered and recovered from COVID-19 has any influence on the medical fitness to dive or the risk of diving accidents.
Novel Corona Virus (SARS-CoV-2) infection (COVID-19) can manifest itself with various clinical syndromes, ranging from no symptoms, over a flu-like syndrome, to severe pulmonary compromise (ARDS – Acute Respiratory Distress Syndrome) and cardiac symptoms (cardiomyopathy). Factors that determine the severity of COVID-19 symptoms are but incompletely known: older persons, suffering from other medical conditions, are an obvious group at risk; also, heavy smokers and obese persons seem to have more risk of complications; however, there are numerous cases reported of young, previously healthy persons in whom the disease has had a sudden and dramatic evolution. In general, if the symptoms were mild and improve within a week to complete resolution, the risk for permanent damage to heart or lungs is very low.
The Board of the SBMHS-BVOOG, after examining the relevant and available literature and discussion with several experts, recommends:
1. Risk of spreading COVID-19: a person who has had symptomatic COVID-19 can, just as someone who was infected but did not have symptoms, spread viral particles in nasal or oral secretions for a certain period after recovery, and thus, still be contagious to others. The exact period during which this is possible is not known and probably variable, but has been reported to be up to 37 days or longer. This is an important consideration for the possible sharing of breathing regulators (buddy-breathing) but also for rescue actions in case of a diving accident.
Therefore, it is recommended:
- That divers who have had symptomatic COVID-19, wait a minimum of TWO months, preferable three, before resuming their diving activity.
- That divers who have tested positive for COVID-19 but have remained completely asymptomatic, wait ONE month before resuming diving.
- Divers who have never had symptoms and have not been tested (who either have not been infected or have had the infection completely asymptomatic) may not have developed immunity against the disease (currently, serological tests are not widely available and do not confirm with 100% certainty a sufficient level of immunity). Therefore, they may still be infected by other divers and would need to observe a waiting period after the release of the confinement period. The duration of this waiting period may be variable depending on the local situation (type of diving, location and local organization).
- Divers and dive centers should observe strictly the guidelines for disinfection of diving gear (as issued by the diving Federations and DAN Europe).
- Risk for pulmonary overpressure syndrome (lung barotrauma): a person who has had COVID-19 infection with severe pulmonary symptoms may suffer from prolonged or even permanent pulmonary damage, even if the lung function seems to have returned to (near) normal. This damage may give a higher risk for lung barotrauma, even after dives without a rapid or uncontrolled ascent. Therefore, it is recommended that a diver who has been hospitalized with or because of pulmonary symptoms in relation to COVID-19, should, after the three-month waiting period (as indicated above), undergo complete pulmonary function testing as well as a high- resolution CT scanning of the lungs. Pulmonary function testing should include FVC, FEV1, PEF25-50-75, RV and FEV1/FVC), and the CT scan should show a return to normal, before resuming diving. It is important that these tests should be interpreted and validated by a medical officer with specific knowledge of diving medicine. If major pulmonary symptoms have been present, even if not requiring hospitalization, pulmonary damage may have occurred and a pulmonary function testing and CT-scan are useful tests.
3. Risk for cardiac events: in the context of general illness and severe pulmonary infection, a COVID-19 cardiomyopathy may not be a prominent symptom and may even go unnoticed during the acute phase of the disease. This however may be the cause of heart muscle damage and subsequent scarring. Cardiomyopathy or cardiac scar tissue may be an important factor in the occurrence of sudden cardiac failure and sudden death during diving immersion. Therefore, it is recommended that a diver who has been hospitalized with or because of cardiac or pulmonary symptoms in relation to COVID-19, should, after the three-month waiting period (as indicated above), undergo cardiac evaluation with echocardiography and exercise test (exercise electrocardiography) to ascertain normal cardiac function. If major pulmonary symptoms or extreme fatigue/exhaustion have been present, even if not requiring hospitalization, this may indicate a possible cardiomyopathy and cardiac testing is useful.
4. Pulmonary oxygen toxicity: at this time, there is very little known as to a possible increased sensitivity of the pulmonary tissue to the toxic effects of oxygen; therefore, a prudent attitude would be that technical diving (with prolonged breathing of hyperoxic gas, with a pO2 of 1.3 ATA or higher) should be avoided. Simple “nitrox” diving (whereby a maximum pO2 of 1.4 ATA is only breathed for short periods, at the deepest part of the dive) should not present any problem.
5.Decompression sickness: even less is known about the possible alteration of the “bubble filter” function of the lung after COVID-19 pulmonary infection. This may imply that the risk for decompression sickness could increase significantly. It has been shown that after deeper recreational dives (close to the No-Decompression-Limit – NDL – of the dive computer, or with mandatory decompression stops), in 70-90% of cases, inert gas bubbles can be detected. These bubbles circulate in the venous blood, and are filtered out by the pulmonary capillary circulation and thus usually do not cause decompression sickness. If the lung “bubble filter” would become less efficient, these bubbles could pass into the arterial circulation (“arterialize”), comparably to divers with a Patent Foramen Ovale, and cause cerebral, vestibular or other types of decompression sickness. Therefore, a prudent attitude would be that divers who have suffered from pulmonary symptoms of COVID-19, limit their dives temporarily (or definitively) to well within the NDL of their computer (so that at no moment during the dive, the computer indicates mandatory decompression stops).
These recommendations are very sensible and should help guide us while we await more data. If a diver suffered a mild case of COVID-19 and is now back to jogging 5 miles per day without issues, he or she can probably return to diving without restrictions or further testing. However, if a diver had a prolonged ICU stay from the infection, especially if they required intubation, maybe they should have follow up CT scans showing resolution of the changes and maybe even pulmonary function testing and echocardiography prior to resuming diving. Only time — and, more importantly, DATA will tell.
What does this all mean? We are in the midst of a generation-defining pandemic the world has not seen in 100 years. There is an appropriate amount of fear and uncertainty gripping the planet. Along with everyone else, we in the diving industry are concerned as to what the long-term effects of this pandemic will be on our livelihoods and the sport we all love.
First of all we need to make sure our sport is safe for our students, our certified divers, and for ourselves. This means changing disinfecting policies, changing some aspects of training, and allowing for social distancing in our dive centers, our dive charters, etc. The best advice at the moment is for any diver who has had a symptomatic case of COVID-19 to be examined by a physician with diving knowledge prior to resuming diving.
As for myself, I am one of the lucky ones. My symptoms of COVID-19 were no worse than a bad case of the flu. I had a normal chest x-ray, normal oxygen saturations, and never had symptoms of shortness of breath. After about two weeks, all of my symptoms resolved and my exercise tolerance on my home rowing machine was back to baseline. I am looking forward to slowly getting back to scuba diving sometime in the next few weeks.
Be safe, everyone. We will come out the other side of this – hopefully as better people in better nations, and living in a better world.
I would like to thank Divers Alert Network and the long list of diving educators, dive instructors, training agencies, and equipment manufacturers whose edits and input helped me put this paper together.

Douglas Ebersole, MD is an interventional cardiologist at the Watson Clinic LLP in Lakeland, Florida and is the Director of the Structural Heart Program at Lakeland Regional Health, an 850-bed tertiary referral hospital in Lakeland. He has been diving since 1974 and is an avid recreational diver, technical diver, rebreather diver, and cave diver. He is also a recreational, technical, and rebreather instructor for several training agencies, is a cardiology consultant to Divers Alert Network, and is the Florida Sales agent for KISS Rebreathers.


